


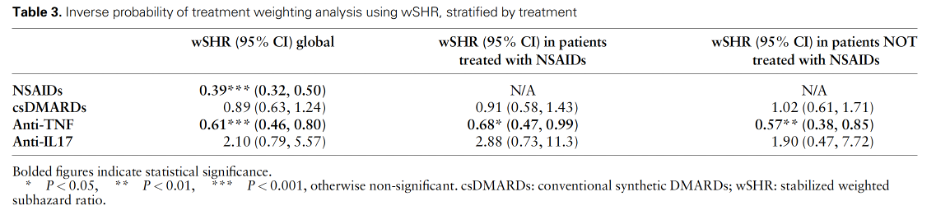
This study by Fakih and colleagues used data from the National Healthcare Data System of France to study risk of major adverse cardiovascular events (MACE) among people with ankylosing spondylitis (AS). The primary findings are reduced risk (hazard) of MACE with NSAID treatment (HR 0.39) and TNF-inhibitor treatment (HR 0.61), which would suggest that these two medication classes protect against incidence MACE.
However, the findings of this study must be interpreted with some caution. Specifically, it is important to note some study limitations related to the individuals whose data included in the present study, and limitations of the data itself. Firstly, included individuals were all beneficiaries in the Long-Term Illness (LTI) Scheme, which required "severe" AS, and may not have captured those whose disease was controlled with NSAIDs alone. Therefore, findings from this work may not be generalizable to individuals with mild AS who are using over-the-counter NSAIDs or who are not part of the LTI scheme. The dataset itself did not include information on over-the-counter/general sales NSAID use, nor did it include specific data on disease severity or activity.
Therefore, while investigators accounted for potential confounding by indication (an higher probability of medication treatment among persons with more severe disease) by constructing a propensity score for treatment, and inverse probability of treatment weighting, this approach is imperfect because of limitations in the data. Finally, overall rates of MACE were lower than expected. Considering the limitations in the study methods and data, and taken together with other publications, these findings are somewhat reassuring that risk of incident MACE is not increased among those with AS who are treated with prescription NSAIDs or TNF inhibitors.
These findings support the hypothesis of a cardioprotective effect of NSAIDs, which is consistent with recent evidence from a Canadian study (Haroon NN et al). The reduced risk with use of TNFi was also reported by an Australian study (Lee JL et al). As with any administrative dataset, clinical details of disease activity and the evaluation of comorbidities was limited. Patients receiving any dose of NSAID were selected, whether it was being used continuously or on demand, and over the counter use could not be addressed. The surprising lack of effect of IL17i therapies may reflect differences in anti-inflammatory mechanisms. I counsel patients about the impact of poor disease control on cardiovascular outcomes and the importance of adherence to therapy.